What is Medical Necessity?
Establishing Medical Necessity
Properly trained and licensed healthcare professionals, such as Doctors of Chiropractic, can diagnose and develop a treatment plan for their patients. Their decision-making skills allow them to determine the frequency of the patients’ visits and what services the patients will receive. As long as the doctor exercises good judgement and meets or exceeds the standard of care, all of the care is clinically appropriate. However, not all care meets the definition of medically necessary. The definition of medically necessary care varies from payer to payer. They establish the definition.
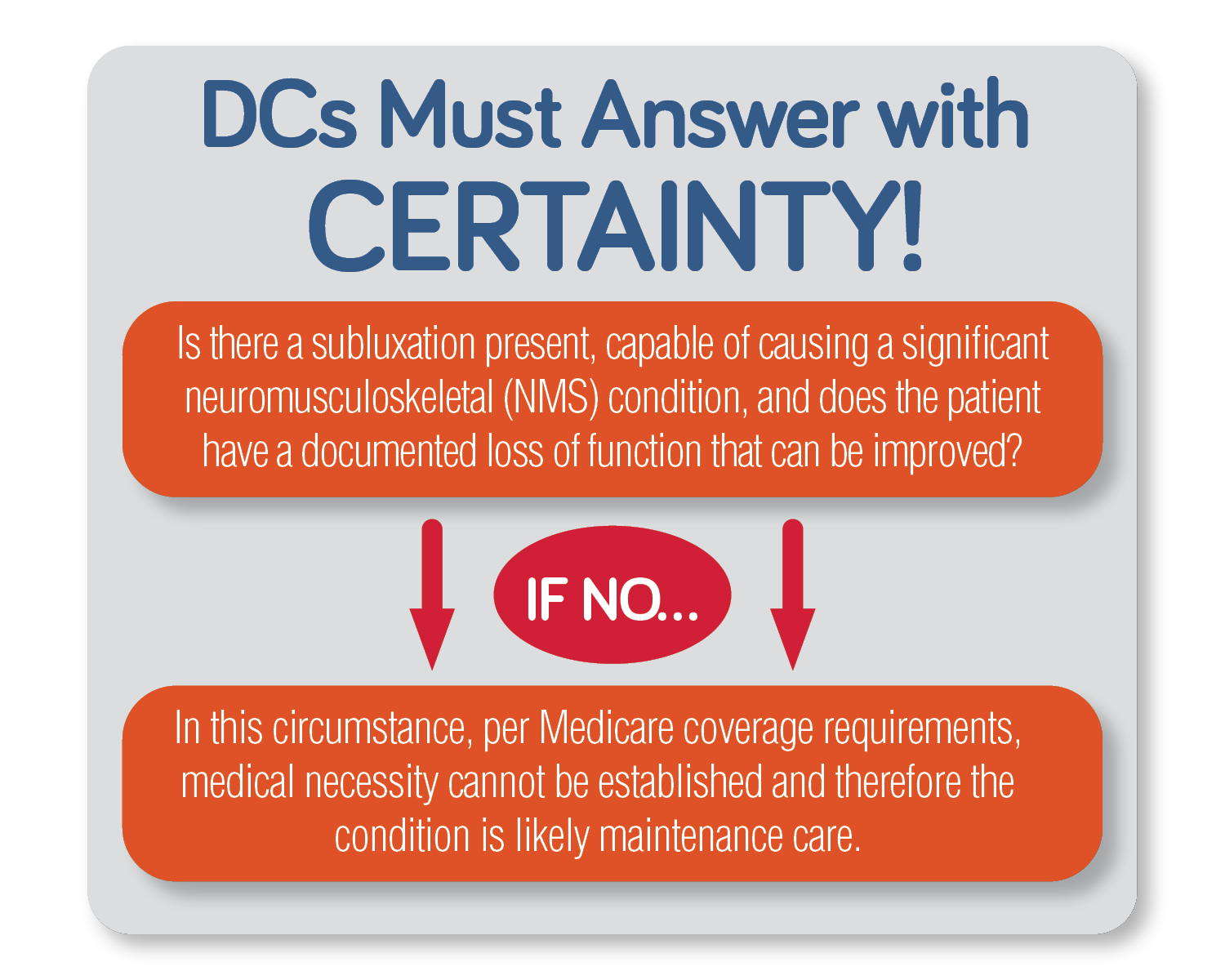
For Medicare, there must be a documented spinal subluxation that is causing a neuromusculoskeletal condition. The ability to improve the patient’s function through treatment is also a requirement. The best way to prove medical necessity is through the provider’s documentation which includes the initial intake, history, exam, daily treatment notes, a treatment plan with measurable functional goals, and possibly imaging. When medical necessity is established, it is called active treatment in Medicare and is designated with an AT modifier when billing. The patient’s care is deemed maintenance care when these criteria are not met. Only spinal manipulations deemed active treatment are payable by Medicare.