Proper Patient Case Management
The Case Management Picture
Case management has its roots in the patient’s clinical presentation and the doctor’s training and expertise. Doctors have a fiduciary responsibility to evaluate patients and determine the whole clinical picture to the best of their ability.
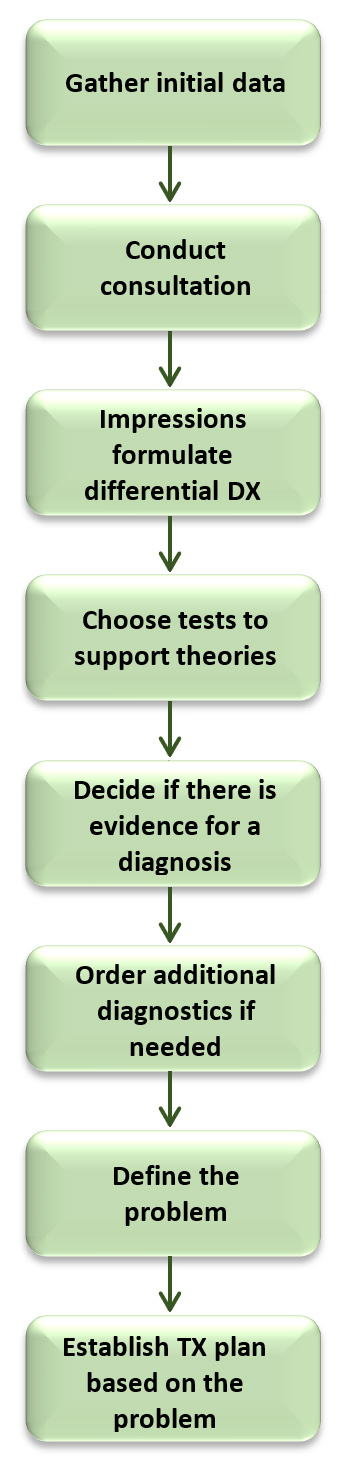
The patient evaluation process is quite linear. The doctor begins by gathering the patient’s history and documenting the chief complaint and then s/he follows the patient’s lead. The rest of the journey might look something like the following. The doctor must follow the steps illustrated on the right.
-
- Initial data is gathered via patient paperwork that details his/her previous medical history, or through a short interview conducted by a team member. Ideally, the doctor reviews this data before meeting with the patient for the first time to get a sense of the direction s/he wants to take during the patient interview process.
- Once the history is established, the doctor follows-up with a more in-depth consultation, asking general health questions, conducting a review of systems, and completing a thorough evaluation of the chief complaint including Onset, Provocation/Palliation, Quality, Region/Radiation, Severity, and Time.
- After the doctor has completed the history and consultation, s/he begins to formulate a differential diagnosis. Now, these impressions and the history must drive the examination choices. Based on the doctor’s conclusions about the patient’s condition, s/he selects proactive orthopedic and neurological tests to prove or disprove those theories.
- When all of the facts about the patient’s physical findings are gathered, the doctor must determine whether there is enough evidence for a conclusive decision about a diagnosis, or if further diagnostic tests are necessary.
- The definition of the problem (or the diagnosis of the condition/subluxation) is defined.
- A written treatment plan/solution to the defined condition is established.
The treatment plan should include details of the doctor’s recommendations including tissue-specific solutions for the patient’s presenting problem. It is especially important to define the functional deficits that will be addressed through this treatment plan and the functional goals that are targeted in order to achieve a specific result from this treatment when a third-party payer is involved.
The doctor should present the patient with a verbal report of his/her:
-
- Findings
- Recommendations
- Expected outcomes from the treatment plan
- Any other options the patient may have (including taking no action at all)
The doctor should inform the patient of the probable outcomes for each of those options so s/he can make an informed decision about how to proceed. The discussion should include information about the patient’s financial responsibility, such as:
-
- Billing third-party payers when appropriate
- Legal means for assistance with payment plans
- Indigence policies
- Professional courtesy policies
The intention is to be sure that the patient is clear about the recommendations and to support the patient as you move forward with the recommended care. Remember, the patient always has the right to refuse treatment. If you do a good job of explaining your recommendations, any alternatives, and the potential outcomes for those alternatives including taking no action at all, your patient will feel confident making the decision to proceed.
Usually, patients choose the doctor’s best recommendation. Once the patient has agreed to proceed with a course of care, the doctor is responsible for helping the patient successfully complete that care. Patients that follow through with the recommendations nearly always recover and stay well, and that is the most satisfying part of practice!