Proper Use of Code S1001- Luxury Item, Patient is Aware
Luxury Item - Patient is Aware
Providers that participate with various third-party payers often find that although verification confirmed coverage for orthotics, the allowable fee schedule agreed to by contract may be lower than the cost of the Durable Medical Equipment (DME) item dispensed. In the case of orthotics, for example, the fee schedule may allow $98/pair, but the orthotics cost $150/pair. The fee schedule doesn’t allow for even a minimal profit on this or any other fixed cost of the provider.
Participating providers may be able to use the HCPCS code S1001 – Deluxe item, patient aware (listed in addition to the code for basic item.) If appropriate and with advanced patient notice and agreement, the patient can opt for the higher level, luxury item (e.g., a Foot Levelers’ Orthotic) and agree to pay the difference between the allowed amount and the provider’s actually charged fee.
Every provider agreement is different; however, we believe that the components of the HIPAA Omnibus Updates published in 2013 clearly allow a patient to direct how a provider deals with the carrier. Figure 1 below is an example of a provider agreement with language explaining that an arrangement between a patient and the provider is permitted. This arrangement should allow the patient to use insurance benefits toward the total cost of the orthotics, then, with agreement upfront, pay the difference between that amount and the provider’s actual fee.
Fig. 1
If you want to consider occasionally using the S1001 billing option, we recommend taking the following steps:
-
- When verifying orthotics coverage with the orthotics verification form, confirm the allowed fee for the item, if possible. Always ask about coverage for S1001 during verification in case it’s necessary to utilize this strategy for your patient to obtain some benefit for the orthotics.
- Check with your Provider Relations Department for any carriers with which the provider has a contract. Find out whether S1001 usage is addressed in the agreement or in the medical review policies. If possible, get all the answers in writing.
- Consider writing to the Provider Relations Department to request an amendment to your agreement with them to permit billing for upgraded products that include advanced-notice cost-sharing with the patient. A letter with sample language can be found in this module.
- Create an Advanced Notice document for the patient to sign. Outline the details and include the circumstances, the products, and the costs. Have this available for your patient to review and okay prior to charging anything above the allowed amount and billing the S1001 code to the carrier. A sample Acknowledgement to Self-Pay form is available in this course in the sample forms provided. (Keep in mind that some payers have their own Advance Notice document, check online first)
- Submit the billing to the carrier using the correct HCPCS codes and amounts as in any other billing situation. Include the S1001 code on the same date of service with a .00- or .01-dollar amount charged (this amount depends on the requirements of your software or electronic billing service). See Figure 2 below for an example.
- Collect the correct amount from the patient reflecting the difference between the actually charged fee and the amount paid by the carrier.
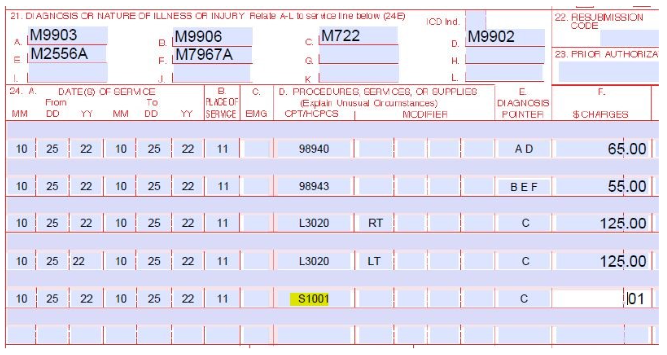
Fig. 2