Supporting CPT® Codes & Modifiers
Code Utilization When Dispensing Orthotics
Coding for functional orthotics is specific to the type of custom orthotic ordered. However, the orthotics may not be the only item in conjunction with the prescription from the provider. In order to accurately describe all the work provided that is associated with orthotic prescription, other codes and modifiers are important. This page outlines the supplementary information necessary for proper coding and billing protocols.
Physical Medicine Codes
The following service codes may be appropriate to include with your patient care when ordering and dispensing orthotics. Coding conventions and rules apply to these codes and often are variable depending on the payer. These codes are included on the suggested verification form so they may be confirmed for coverage. Also, some payers require modifiers on these codes since they fall into the physical medicine section of the CPT® coding book. They are outlined below.
CPT® Code 97760: Orthotic(s) management and training (including assessment and fitting when not otherwise reported), upper extremity(s), lower extremity(s) and/or trunk, each 15 minutes
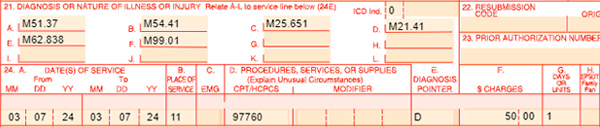
This service may be rendered and billed the day the functional orthotics are dispensed to the patient and may only be used for “custom fabricated” supports. This code includes the fitting of the functional orthotics, training in their use, care, and wearing time of the functional orthotics and brief instructions in exercises while the functional orthotics are in place. Direct one-on-one contact by the provider of service is required and is timed-based for billing. You need to properly document the time spent in your daily note. Combine the treatment time for any other time-based codes on the same encounter and code according to the time-based coding information in this module. Here is an example of billing for this code. Notice the specificity of the diagnosis pointer in box 24E.
CPT® Code 97763: Orthotic(s)/prosthetic(s) management and/or training, upper extremity(ies), lower extremity(ies), and/or trunk, subsequent orthotic(s)/prosthetic(s) encounter, each 15 minutes
This service is intended for established patients who have already received their functional orthotics. It is essential for the healthcare practitioner to follow-up with a patient after they have been provided with a pair of functional orthotics. The “checkout” visit would include assessing the patient’s response to wearing functional orthotics such as possible skin irritation or breakdown, determination if the patient is donning the functional orthotics appropriately, need for padding, under wrap or socks, and tolerance to any dynamic forces being applied. This code requires direct one-on-one contact by the provider and is timed-based for billing. You need to properly document the time spent in your daily note. Combine the treatment time for any other time-based codes on the same encounter and code according to the time-based coding information in this module.
Modifiers
Modifiers, when appended to a billing code, indicate that a service or procedure performed has been altered by some specific circumstance but not changed in its definition or code. They are used to add information or change the description of the service to improve accuracy or specificity. In recent years, more modifiers are required when billing physical medicine codes. More and more payers require these codes when billed by any provider type. The following table outlines the most common modifiers that are used with these codes. Review the CMS 1500 billing form samples for real-time uses of these modifiers.
| Modifier | Description | Used with Which Codes |
| 96 | Used on codes when such services help an individual learn skills and functioning for daily living that the individual has not yet developed and then keep or improve those learned skills. Habilitative services also help an individual keep, learn, or improve skills and functioning for daily living. | Physical Medicine Codes by Payer Mandate |
| 97 | Rehabilitative services help an individual keep, get back, or improve skills and functioning for daily living that have been lost or impaired because the individual was sick, hurt, or disabled. | Physical Medicine Codes by Payer Mandate |
| GP | The GP modifier indicates that a provider’s services have been provided in conjunction with a physical therapy plan of treatment. Many payers require this modifier on any physical medicine code, but it’s always required when billing Medicare. | Physical Medicine Codes by Payer Mandate |
| RT/LT | Used to indicate the side of the body on which a service or procedure is performed. In the case of functional orthotics, it’s used on each line item to indicate that two orthotics are dispensed. | L-Codes for Orthotics |