Billing Orthotics to Third-Party Payers
Identify & Follow the Requirements
Practices that dispense and bill Durable Medical Equipment (DME) to third-party payers must pay close attention to the billing requirements of the carrier being billed as they often vary from carrier to carrier. Several factors come into play when billing directly to third-party payers:
-
- What diagnosis codes are considered medically necessary, and therefore payable, according to the carrier’s Medical Review Policy (MRP)? Is the diagnosis/condition the doctor assigned for your patient included?
- Are the billing codes that describe the orthotics your office dispensed listed in the MRP as covered billing codes?
- After verifying the patient’s third-party coverage, are orthotics a covered benefit? If so, how often can they be dispensed and paid for by the carrier?
- Will the carrier pay for more than one pair of orthotics in a period of time?
- Do you know the allowable fee for the orthotics according to the provider fee schedule? If so, is it going to cover the cost of the orthotics?
- Does the carrier you’re billing require that a certified DME provider or company bill all DME? If so, are you considered this type of provider? If not, there may be no coverage for the patient for DME dispensed directly by the doctor.
In general, there is no additional code to bill for the foot scan. The scan is usually conducted on the same date as any other Evaluation and Management (E/M) service. If it isn't, the cost is bundled into the cost of the orthotics themselves in most cases.
Billing orthotics on your CMS-1500 billing form is not very different from billing other services. Figure 1 shows an example of the billing section of the form and how it might look if billing, along with the other services from the initial visit. Notice that one pair of customized, functional orthotics was prescribed and ordered for a total actual fee of $300 for the pair. The bill includes both the left and right orthotic, and each line item represents one unit of the pair. Pay special attention to the diagnosis pointing in box 24E of the billing form, identifying only the diagnoses that apply for the service rendered.
(Example provided for educational purposes only)
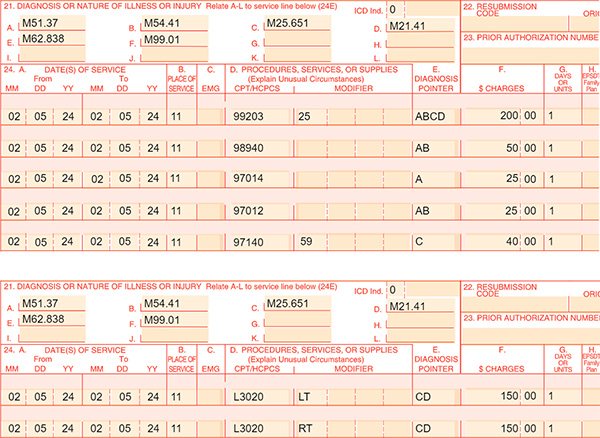
Fig. 1
You can review the sample initial visit documentation for this sample date of service by clicking HERE.
If the carrier’s allowance included coverage for two pairs of customized, functional orthotics and each pair costs $300.00, Figure 2, below, illustrates how billing might differ. Notice that each line item represents two units each for the left and right orthotic, for a total of two pairs.
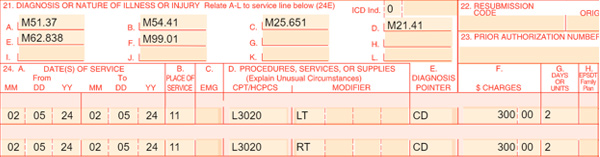
Fig. 2
It’s important to understand the meaning of a Medically Unlikely Edit (MUE). An MUE is a Medicare unit of service claim editapplied to healthcare claims against a procedure code for services rendered by one provider/supplier to one patient on a single day. An MUE for an HCPCS/CPT code is the maximum units of service that a provider would report under most circumstances for a single beneficiary on a single date of service. Commercial carriers sometimes use these edits to screen for unlikely circumstances that should not be paid (e.g., It may be unlikely to dispense two pairs of orthotics to the same patient on the same day.) The edit might capture the service and automatically deny it, but if the coverage has been verified, and it allows for two pairs, and they are medically necessary, don’t hesitate to appeal the denial. The documentation in the patient’s clinical record should reflect the medical necessity for more than one pair and outline the details needed to justify the order.