CMS issued the CY 2026 Physician Fee Schedule (PFS)
This final rule announces policy changes for Medicare payments under the PFS and other Medicare Part B issues. Historically CMS utilized the AMA RUC to estimate practitioner time, work intensity and other expenses when evaluating codes paid. Starting in 2026 we will see two separate conversion factors. Future fees will most likely rely on the Medicare Economic Index (MEI) productivity adjustment percentage. The goal is to address distorted payment values.
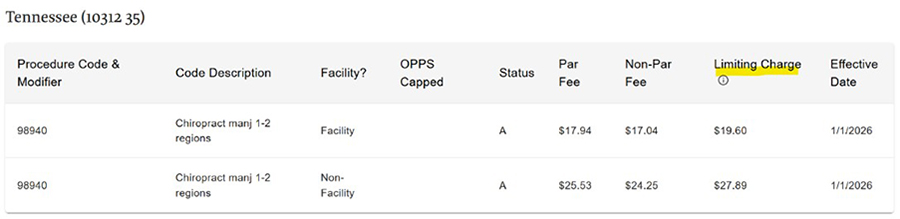
Reduce confusion and frustration by locating your fees for your jurisdiction. Take time to update your practice management software with the information provided by your local MAC by January 1, 2026.
Providers who are out of network with Medicare Advantage (MA) Plans will want to pay close attention to the rules that surround MA plans. In most cases, out of network doctors are restricted to billing the self-pay patient the CMS amount listed as the Limiting Charge. Be sure to update your billing procedures with this information.
Learn about the PFS Look Up Tool at: https://www.cms.gov/medicare/physician-fee-schedule/search/overview
Search your fees at: https://www.cms.gov/medicare/physician-fee-schedule/search
The other option is to locate the Fee Schedules on your local MAC website.
Some examples are listed below:
Palmetto GA: https://palmettogba.com/jjb/did/avgkpw7730
CGS: https://www.cgsmedicare.com/partb/fees/index.html
Noridian: https://med.noridianmedicare.com/web/jeb/fees-news/fee-schedules/mpfs